Generic
Ototoxicity: How Certain Drugs Can Affect Your Hearing and Balance
By Team Hearzap | Dec. 15, 2025
Medicines save lives, yet a small group can irritate the inner ear. When that happens, hearing, balance, or both can change. This effect is called ototoxicity. If someone in India is being treated for cancer, tuberculosis, serious infections, or heart or kidney disease, it helps to understand ear-related side effects early. This guide explains what is ototoxicity, gives an ototoxicity definition, lists key medicines and shows steps to protect you during treatment. If you have seen the misspelling ototoixcity, it refers to the same issue.
What Is Ototoxicity? (Meaning, Definition & Overview)
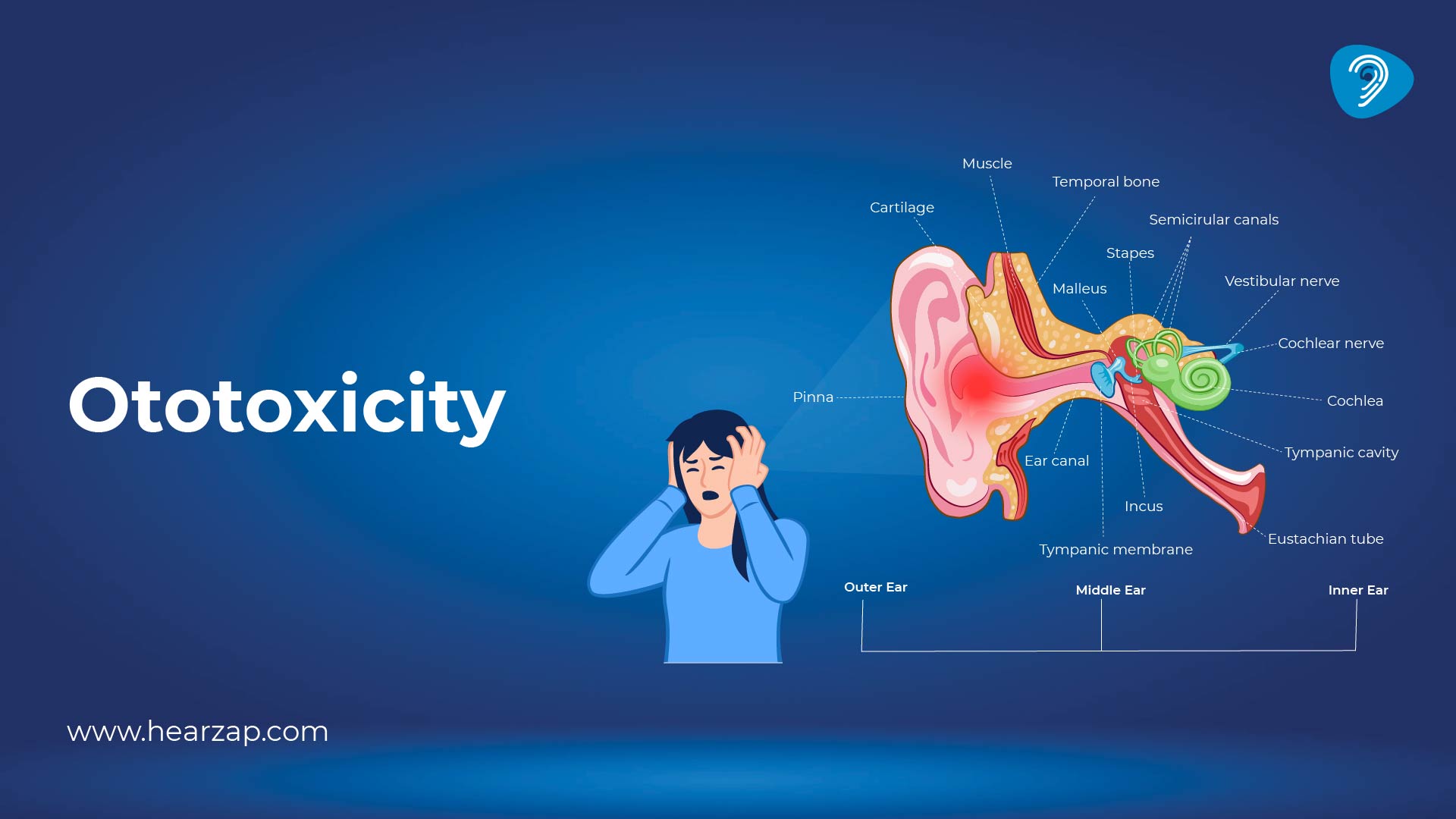
In plain words, the ototoxicity meaning is medicine-related harm to the inner ear that affects hearing or balance. The formal ototoxicity definition is damage to the cochlea, the auditory nerve, or the vestibular system from a drug or chemical, causing a measurable change in hearing or balance. What is ototoxicity for a patient? A necessary medicine begins to create ear-related effects that you can feel or that tests can detect, even before daily listening becomes hard.
Medical Definition of Ototoxicity
Clinically, injury is grouped by the structure involved. Cochleotoxicity means damage in the cochlea, often starting at the outer hair cells that detect high-pitched sounds. Vestibulotoxicity affects the balance organs. Some medicines irritate both, so a person may notice ringing and feel unsteady.
How Ototoxicity Affects the Ear and Balance System
Hair cells in the cochlea convert sound into electrical signals. Some medicines create oxidative stress here, so cells malfunction or die. That is cochleotoxicity. In the vestibular system, similar stress affects balance hair cells, causing blurred vision with head movement, a floating sensation, or falls. Risk rises with kidney disease, dehydration, and when more than one ear is affected by the medicine.
Common Ototoxic Drugs You Should Know About
Several medicine groups carry risk. The term ototoxic drugs does not mean they are unsafe for everyone. It means the benefit must be balanced against the risk, and you should be monitored. Major groups include:
- Chemotherapy agents such as cisplatin and carboplatin.
- Loop diuretics like furosemide and bumetanide for heart or kidney conditions.
- Salicylates in high doses, for example, aspirin overuse.
- Antimalarials such as quinine derivatives.
- Some antivirals and anti-tuberculosis drugs.
Review your prescription list with your doctor.
Antibiotics Linked With Ototoxicity
Aminoglycoside antibiotics, used for severe infections and sometimes for drug-resistant tuberculosis, are well known. Gentamicin, amikacin, tobramycin, kanamycin, and streptomycin can injure inner ear cells. Risk rises with higher doses, longer courses, kidney disease, or when combined with other ototoxic drugs. When such antibiotics are essential, doctors arrange baseline and periodic ear checks to catch changes early.
Symptoms and Early Signs of Ototoxicity
Ototoxic effects can be subtle at first. You may feel fine one day and then notice small changes the next week. Watch for the signs of ototoxicity and tell your care team promptly.
Hearing-Related Symptoms
- Ringing, hissing, or buzzing in one or both ears. Some people hear a pulsing sound that matches the heartbeat, called pulsatile tinnitus.
- Difficulty following speech in a busy market or office.
- Muffled perception of high-pitched sounds like birds or children’s voices.
- A need to turn up the volume more than before, which may indicate hearing loss.
Balance-Related Symptoms
- Spinning spells, especially when turning the head or rising from bed.
- Rocking or swaying makes straight-line walking harder.
- Blurred vision during quick head movement.
These can overlap with non-ear causes of vertigo.
Causes of Ototoxicity: Why Do These Drugs Affect Your Hearing?
There are several causes of ototoxicity, and most act together:
- Direct injury to hair cells through reactive oxygen species.
- Reduced blood flow to the inner ear during rapid infusion or dehydration.
- Accumulation of the drug when the kidneys or liver are not clearing it well.
- Genetic variations that make the inner ear more sensitive.
- Combined use of more than one medicine that affects the ear.
Drug Dosage & Duration
Higher total dose and longer duration increase risk. Rapid intravenous injection can create peaks that the ear cannot tolerate. Doctors reduce risk through careful dosing and, where possible, drug level monitoring. Do not change doses yourself.
Pre-existing Hearing Conditions
People with existing ear problems are more vulnerable. That includes those with chronic ear disease, older adults, and children. Noise exposure adds strain. If you already know your types of hearing loss, share that report before starting high-risk therapy.
Genetic Susceptibility
Some people carry mitochondrial variants that make inner ear cells sensitive to aminoglycosides. A family history of deafness after antibiotic use is a clue. Genetic tests are available in select centres, but even without testing, close monitoring helps.
How Ototoxicity Is Diagnosed
Diagnosis starts with history, a medicine review, and an ear examination. You may be referred to an ENT specialist and an audiologist for tests. Baseline testing before treatment makes change easier to spot.
Ototoxicity Audiogram & Hearing Test Process
The ototoxicity audiogram uses high-frequency pure tone hearing test methods along with standard audiometry. Baseline thresholds are recorded, often beyond 8 kHz. Speech tests, otoacoustic emissions, and tympanometry may be added. If a change is detected, the team weighs the benefit against the risk and may adjust the plan.
Vestibular Testing for Balance Issues
If balance is affected, the clinic may use video nystagmography, a head impulse test, and posturography. These tests are safe and help tailor therapy.
Treatment Options & What You Can Do Next
Plans depend on the medicine, the illness, and how early the change is picked up. Aim for teamwork between your prescribing specialist and an ENT or audiology service.
Can Ototoxicity Be Reversed?
Some effects are temporary and improve once the drug is stopped or the dose is reduced. High-dose salicylate-related ringing is a common example. Others are permanent, as with cisplatin or many aminoglycosides. Early detection gives the best chance to limit damage.
Monitoring Strategies While Taking High-Risk Medications
- Get a baseline ear evaluation and repeat it during the course.
- Report any ringing, fullness, difficulty in noise, imbalance, or falls right away.
- Stay hydrated and avoid non-prescribed painkillers or herbal mixes.
- If a change appears, ask whether dose, drug, or infusion speed can be adjusted; keep your test results.
Assistive Solutions: Hearing Aids & Balance Therapy
If hearing is affected, modern hearing aids can improve everyday communication and reduce listening effort. For balance problems, vestibular rehabilitation helps the brain adapt. Counselling, safety changes at home, and community support also help.
How to Prevent Ototoxicity: Safe Medication Practices
The goal is safe care, not fear of important medicines. Many people complete life-saving treatment without ear issues when the team plans.
Talk to Your Doctor About Alternatives
Before starting therapy, ask about options, duration, and risk. If a safer alternative exists, your doctor will explain the trade-offs. Do not stop or switch medicines on your own.
Keep Track of Symptoms Early
Maintain a simple diary of any ear sensations, spells of imbalance, or trouble following speech. Share it at each visit.
Regular Hearing Tests for High-Risk Patients
Schedule checks at the start, during treatment, and shortly after completion. Children, older adults, and those with kidney disease or previous ear trouble need closer follow-up. Also, protect your ears from other risks; ear damage from loud noise at weddings or concerts can compound medicine-related stress on hair cells.
When to See a Hearing Specialist
Seek prompt care if you notice new ringing, sudden loss of clarity, repeated falls, or a spinning sensation that lasts longer than a few minutes. An ENT surgeon and an audiologist can assess you and coordinate with your primary specialist.
Conclusion
Medicines that affect the ear are a real concern, but knowledge and planning keep most people safe. Understand the ototoxic meaning, know which ototoxic drugs may be part of your treatment, watch for the signs of ototoxicity, and get the right tests at the right time. With timely monitoring and open conversation, you can complete essential therapy while protecting hearing and balance safely.
FAQs
Does everyone who takes ototoxic medicine develop problems?
No. Risk depends on the drug, the dose, your health, and your genetics. Many people finish treatment without change when monitored well.
What should I do if I notice ringing or imbalance during treatment?
Tell your doctor as soon as you can. Early assessment allows dose adjustments or a change in plan where appropriate.
Are there warning signs I can check at home?
Yes. Watch for trouble following conversations in noise, new ringing, a need to raise the volume, unsteadiness, or blurred vision with head movement.
Can lifestyle changes help while I am on treatment?
Yes. Stay hydrated, rest well, avoid unnecessary medicines, and protect your ears from loud environments.
Contact us
We are here for all your hearing needs, from hearing tests to hearing aids. Fill out the form below, and we will give you a call soon.
Please enter a valid mobile number with 10 digits.
Recent Blogs
By None | Feb. 7, 2026
By None | Feb. 6, 2026
By None | Feb. 5, 2026
By None | Feb. 4, 2026
By None | Feb. 3, 2026