HEARING LOSS
Autoimmune Disorders and Hearing Loss: Is There a Connection?
By Team Hearzap | Nov. 3, 2025
You may know someone who lives with rheumatoid arthritis, lupus, or thyroid disease. These conditions are “autoimmune,” where the immune system mistakenly identifies healthy tissues and cells as invaders and attacks them. When this immune response targets the ear, it can damage the cochlea, auditory nerve, or inner ear blood vessels, disrupting how sound is processed. Over time, that friendly fire can affect more than joints or skin. It can also interfere with the delicate machinery of the inner ear, leading to hearing loss that may be sudden, fluctuating, or progressive. This article covers the science, warning signs, and treatments Indian patients commonly receive.
Understanding Autoimmune Disorders
Autoimmune disorders are a large family of conditions where your body’s defence system becomes overactive or misdirected. Instead of targeting viruses and bacteria, it reacts to your own tissues. There are over 80 recognised illnesses; some are organ-specific (like Hashimoto’s thyroiditis) and others are systemic. Genetics, hormones, infections, environment, and stress all play a role.
Autoimmunity can be lifelong; care aims to control inflammation and preserve function. If you already have an autoimmune diagnosis and notice ear symptoms, seeking an early hearing test is wise because speed matters in protecting the cochlea and auditory nerve.
How the Immune System Affects the Body
When the immune system is dysregulated, it releases inflammatory chemicals (cytokines) and autoantibodies. These can cause:
- Swelling and tissue damage in targeted organs.
- Reduced blood supply to tiny structures such as the cochlea.
- Fluid build-up and pressure changes within the inner ear.
- Increased risk of clotting or vasculitis that starves hair cells of oxygen.
The inner ear is exquisitely sensitive. Even short bursts of inflammation can harm the sensory hair cells that convert sound waves into signals your brain understands. That is why autoimmune flares sometimes present with ear fullness, imbalance, or a sudden drop in hearing that needs urgent attention.
The Link Between Autoimmune Disorders and Hearing Loss
The connection is twofold. First, some autoimmune conditions directly attack ear structures. Second, systemic inflammation or vascular changes make the inner ear more vulnerable to damage from infections, medications, or noise. In clinics across India, ENTs frequently see patients whose first hint of autoimmunity was unexplained hearing loss. Early recognition and coordinated care with rheumatology significantly improve overall outcomes.
Autoimmune Inner Ear Disease (AIED): The Main Culprit
Autoimmune inner ear disease - often shortened to AIED - is the best-known example of autoimmune hearing loss that primarily targets the inner ear. People typically present with:
- Rapidly progressive or fluctuating loss in one or both ears.
- Tinnitus (ringing), a feeling of fullness, and sometimes vertigo.
- Episodes that worsen over weeks, then partly recover.
AIED may exist alone or alongside systemic conditions like rheumatoid arthritis or inflammatory bowel disease. The underlying process involves immune cells attacking inner-ear antigens, with inflammation damaging the cochlea and, at times, the vestibular system. Because early treatment improves the odds of recovery, doctors often use a “diagnose and treat” approach: start medication promptly and monitor for improvement while tests are underway.
Other Autoimmune Conditions Linked to Hearing Loss
While AIED is the classic culprit, several autoimmune illnesses have recognised ear involvement:
- Rheumatoid arthritis: Immune-mediated inflammation, vasculitis, and certain medicines can affect hearing thresholds.
- Systemic lupus erythematosus: Immune complexes and vascular changes may lead to sensorineural loss and tinnitus.
- Hashimoto’s thyroiditis and Graves’ disease: Thyroid imbalance can alter circulation and fluid balance within the ear.
- Cogan’s syndrome: A rare disorder causing interstitial keratitis and vestibulo-auditory symptoms, often with rapid deterioration.
- Vasculitides (e.g., granulomatosis with polyangiitis): Blood-vessel inflammation can impair the microcirculation of the cochlea.
- Psoriasis and psoriatic arthritis: Systemic inflammation is associated with slightly higher rates of auditory symptoms.
Knowing about these links helps you and your clinician act faster if new ear symptoms arise during an autoimmune flare.
Signs and Symptoms of Autoimmune Hearing Loss
Autoimmune ear problems often look different from age-related changes. Common red flags include:
- Sudden drop in hearing in one ear (or both) over hours to days.
- Fluctuating thresholds - better some days, worse on others.
- Persistent tinnitus or a sensation of blocked ears without wax.
- Dizziness, imbalance, or pressure sensations.
- Difficulty following conversations in background noise.
- Ear symptoms that coincide with joint pain, rashes, dry eyes, mouth ulcers, or fatigue.
If you notice any of the above, book a hearing test without delay. Many hospitals in India can arrange same-day audiometry, and most reputable clinics now offer an online hearing test as a quick first step when travel is hard. An online screen isn’t a diagnosis, but it can nudge you to get timely care.
How Is Autoimmune Hearing Loss Diagnosed?
There is no single “AIED blood test,” so doctors rely on a combination of history, examination, and investigations. Expect some of the following:
- Audiometry and speech tests: to map the type and degree of loss.
- Tympanometry: to assess eardrum and middle-ear function.
- Otoacoustic emissions (OAEs): to gauge hair-cell health.
- MRI of the internal auditory canals: if asymmetrical loss or neurological signs are present, to rule out other causes.
- Blood work: full blood count, ESR/CRP, thyroid profile, autoimmune markers (ANA, ANCA, rheumatoid factor), and, depending on symptoms, specific tests requested by your rheumatologist or ENT.
- Trial of therapy: A short course of corticosteroids may be prescribed. Improvement supports an immune-mediated mechanism, though it is not absolute proof.
Bring previous test results, a medication list, and a symptom diary. Note any exposure to loud noise or ototoxic drugs, because these can worsen vulnerability during autoimmune activity.
Treatment Options for Autoimmune-Related Hearing Loss
Management has two aims: calm the immune system and restore or support hearing. Treatment is individualised; your ENT and rheumatology team will weigh benefits and side-effects, especially if you have diabetes, hypertension, or glaucoma.
Common approaches include:
- Hearing technology: Modern hearing aids are small, smart, and can be tuned precisely to fluctuating thresholds. For profound loss, a cochlear implant may be considered after multidisciplinary evaluation. Assistive listening devices (remote microphones, TV streamers) help in classrooms and busy homes.
- Corticosteroids: Often the first-line option for suspected autoimmune hearing loss. They reduce inflammation and may reverse recent damage. Doctors may use oral tablets or, in some cases, intratympanic injections that deliver medicine directly into the middle ear.
- Immunosuppressants or biologics: Methotrexate, azathioprine, cyclophosphamide, or targeted biologics are considered when symptoms recur or steroid doses become difficult to taper. These drugs require careful monitoring.
- Plasma exchange or IVIG: Reserved for complex cases under specialist care, particularly when systemic autoimmunity is severe.
- Lifestyle and comorbidity control: Protect your ears from noise, manage thyroid and lipid levels, and prioritise sleep - chronic stress can worsen flares. A balanced diet and regular movement support vascular health.
Can Hearing Be Restored After Autoimmune Damage?
Sometimes, yes, especially if treatment starts early. Many patients experience partial or even near-complete improvement after steroids or immunotherapy. But outcomes vary:
- Recent, mild losses respond best.
- Long-standing or repeated flares can cause irreversible hair-cell damage.
- Fluctuating patterns may leave gaps in clarity even when thresholds look “normal.”
The encouraging news is that a personalised combination of medical therapy and technology can restore communication in most daily settings. If your thresholds stabilise but clarity remains poor, ask about advanced fittings, speech-in-noise training, and remote-microphone accessories - practical tools that reduce listening effort at work, in lecture halls, and at family gatherings.
Managing Hearing Health with Autoimmune Disorders
Autoimmunity often runs in cycles. The trick is to stay ahead of changes and act promptly during flares. Consider these habits:
- Schedule regular audiology reviews. If you have a systemic autoimmune condition, an annual hearing test or more frequent checks during active disease help catch shifts early.
- Use an online hearing test between appointments. Many hospital groups and hearing centres in India provide reliable screens you can do at home with headphones. Treat them as a nudge to book in-person care if the results dip.
- Keep a symptom and medication log. Note ear fullness, ringing, dizziness, and any changes after dose adjustments.
- Control cardiovascular risks. High blood pressure, diabetes, and smoking are tough on the tiny vessels that feed the cochlea.
- Prioritise noise protection. Carry earplugs for weddings, festivals, and loud workplaces. Avoid stacked exposures, for example, loud gym classes after a day at a construction site.
- Lean on technology. Today’s hearing aids can auto-adjust for restaurants, online meetings, and phone calls. Bluetooth streaming and apps make them easy to use.
When to See a Doctor
Seek urgent ENT care if you notice:
- Sudden hearing loss in one or both ears.
- Severe vertigo with nausea or neurological symptoms.
- Ear symptoms during a known autoimmune flare.
- A recent viral illness or new medicine followed by ear fullness, tinnitus, or imbalance.
For non-urgent concerns, such as gradual difficulty following speech, start with a hearing test. If in-person appointments are hard to arrange, book an online hearing test as a first step and use the report to plan your next visit.
Final Thoughts
Autoimmunity and the ear intersect more often than most of us realise. While autoimmune inner ear disease is the clearest example, many systemic illnesses can trigger autoimmune hearing loss or make your ears more vulnerable during flares. The good news is that prompt treatment, smart technology, and steady habits can preserve connection and quality of life.
If you live with an autoimmune condition, put your ears on the checklist: protect them from noise, track changes, and seek help early. A timely hearing test followed by treatment and, when needed, well-fitted hearing aids can make the difference between struggling through conversations and engaging fully at home, at work, and in every celebration on your calendar.
Related Blogs
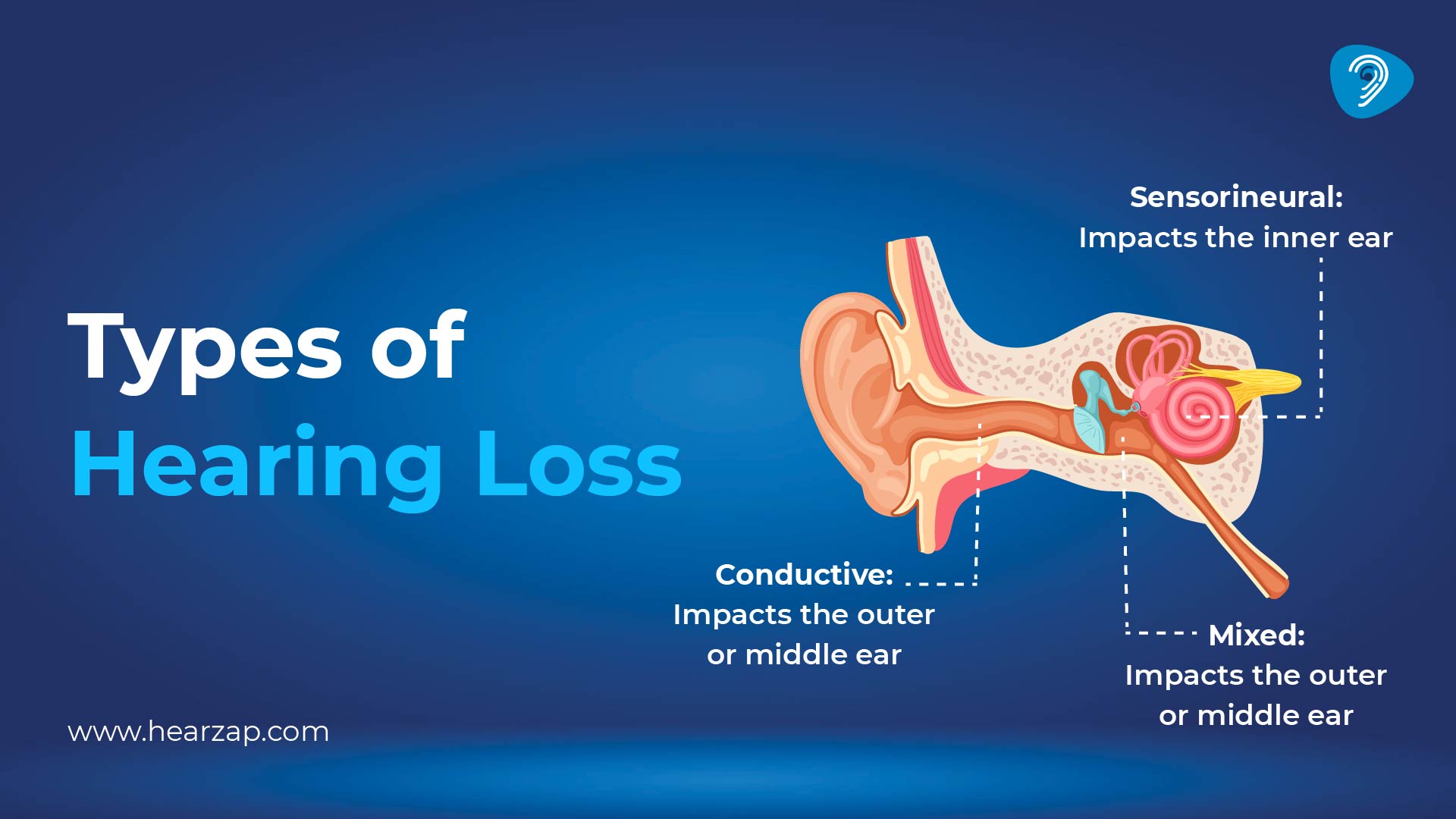
Understanding Types of Hearing Loss

How Hearing Loss Affects Daily Life
Contact us
We are here for all your hearing needs, from hearing tests to hearing aids. Fill out the form below, and we will give you a call soon.
Please enter a valid mobile number with 10 digits.
Recent Blogs
By None | Feb. 16, 2026
By None | Feb. 9, 2026
By None | Feb. 7, 2026
By None | Feb. 6, 2026
By None | Feb. 5, 2026









