Generic
Mastoiditis: Causes, Symptoms, and Treatment Options
By Team Hearzap | Oct. 2, 2025
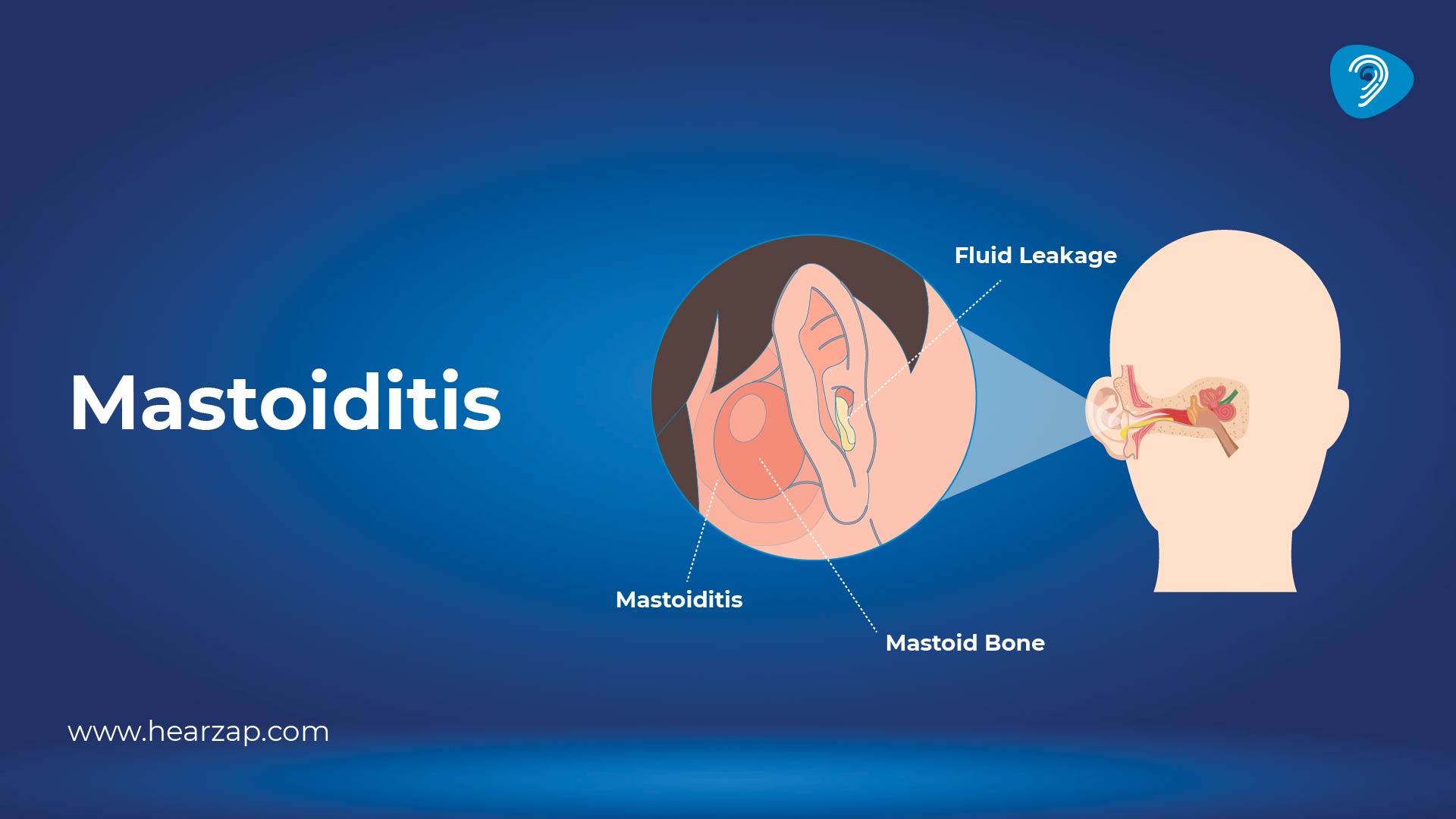
Mastoiditis sounds complicated, but the idea is simple: it is inflammation and infection of the honeycomb air cells in the mastoid bone, the bony bump you can feel just behind the ear. The problem usually follows trouble in the middle ear and needs timely care from an ENT specialist. This guide explains what it is, why it happens, how to recognise it early, and the options your doctor may discuss if treatment is needed.
What is Mastoiditis?
At the back of each ear sits the mastoid bone, which is light and spongy inside. When germs travel from the middle ear into these air spaces, the lining becomes inflamed, and pockets of fluid or pus can collect. In everyday language, mastoiditis is a rare but important complication of ear infection in children and adults. Because the mastoid is close to the ear canal, the eardrum, and the brain, new pain, swelling, or fever after middle ear infections deserves attention. Early evaluation helps prevent the spread and keeps simple problems from becoming complex. Children and adults can be affected.
Mastoiditis Causes
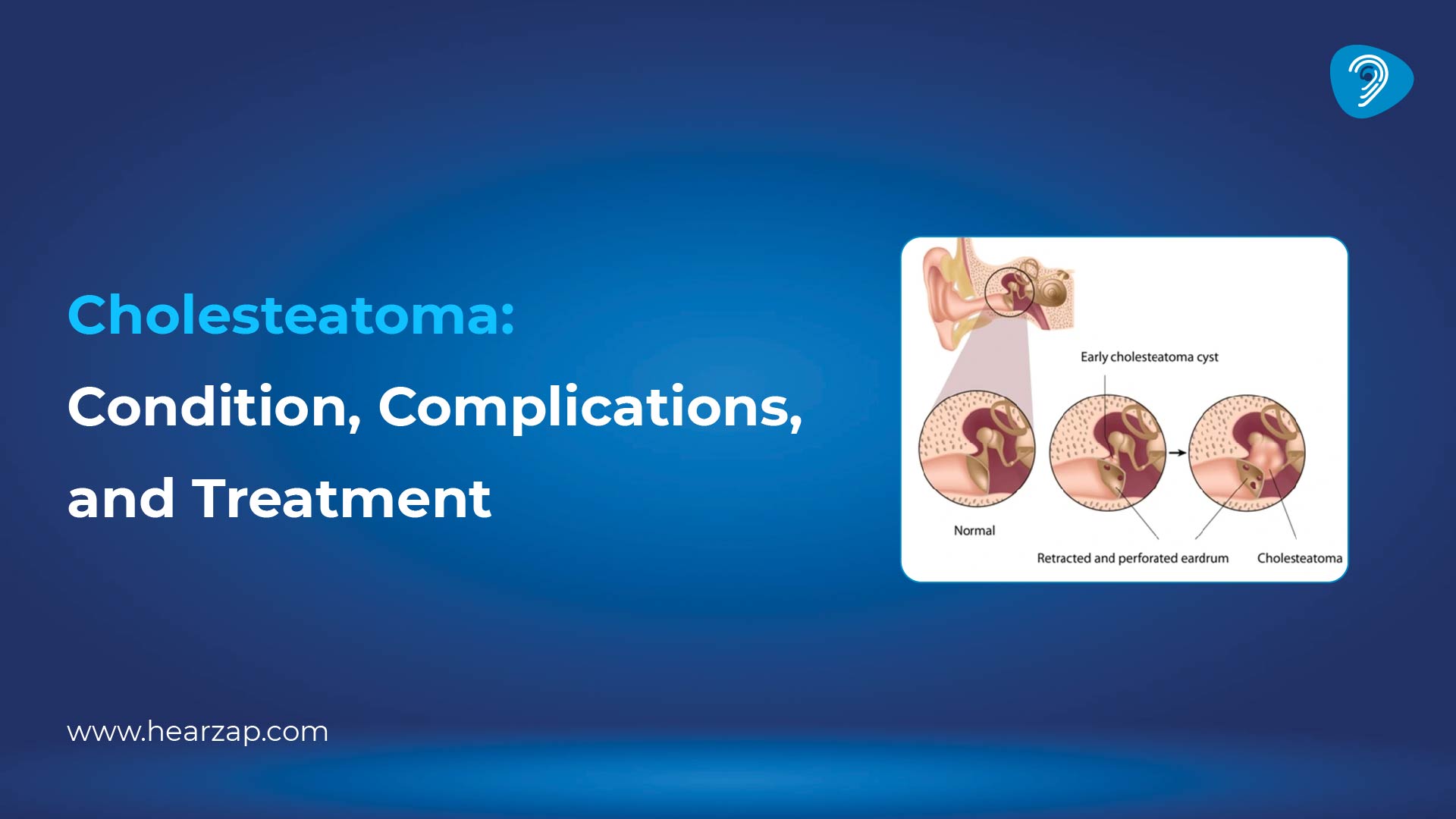
Common mastoiditis causes begin with an ear infection in the middle ear (otitis media). The narrow tube connecting the middle ear to the back of the nose can swell during a cold or allergy flare. Trapped fluid then feeds germs, and pressure builds. If the eardrum does not ventilate well, infection can spread into the mastoid air cells. Less often, skin infections, cholesterol granuloma, or injury to the ear can irritate the area. Factors that raise the chance include repeated middle ear infections, exposure to tobacco smoke, cleft palate, and a weakened immune response.
Signs and Symptoms of Mastoiditis
Knowing the early signals helps you act calmly and quickly. Common mastoiditis symptoms include:
- Deep, throbbing ear pain that may feel worse at night or when lying on the affected side.
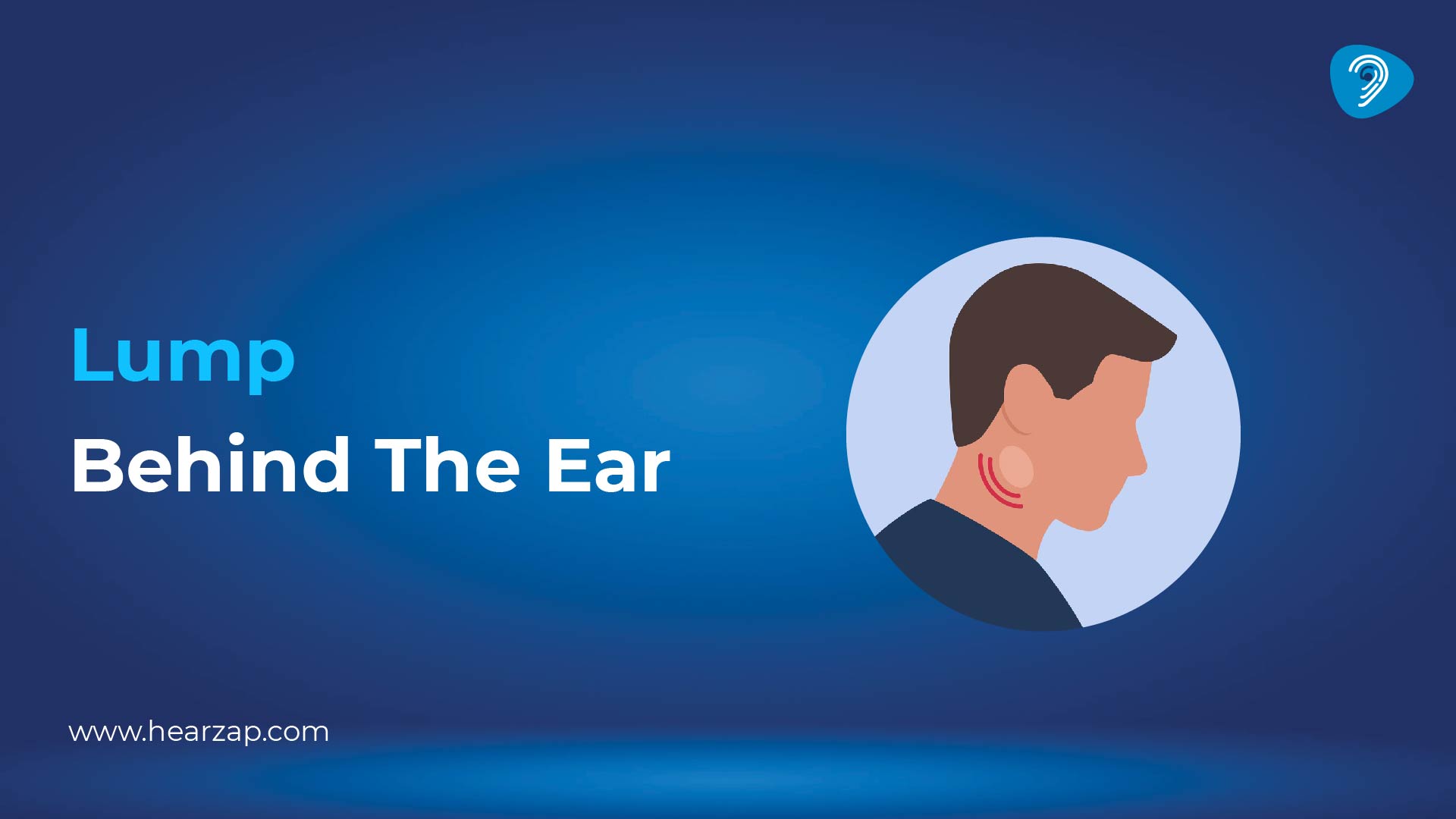
- Tenderness, warmth, or redness behind the ear with swelling that can push the ear outward.
- Fever, irritability in children, tiredness, or reduced appetite.
- New ear discharge after a recent ear infection.
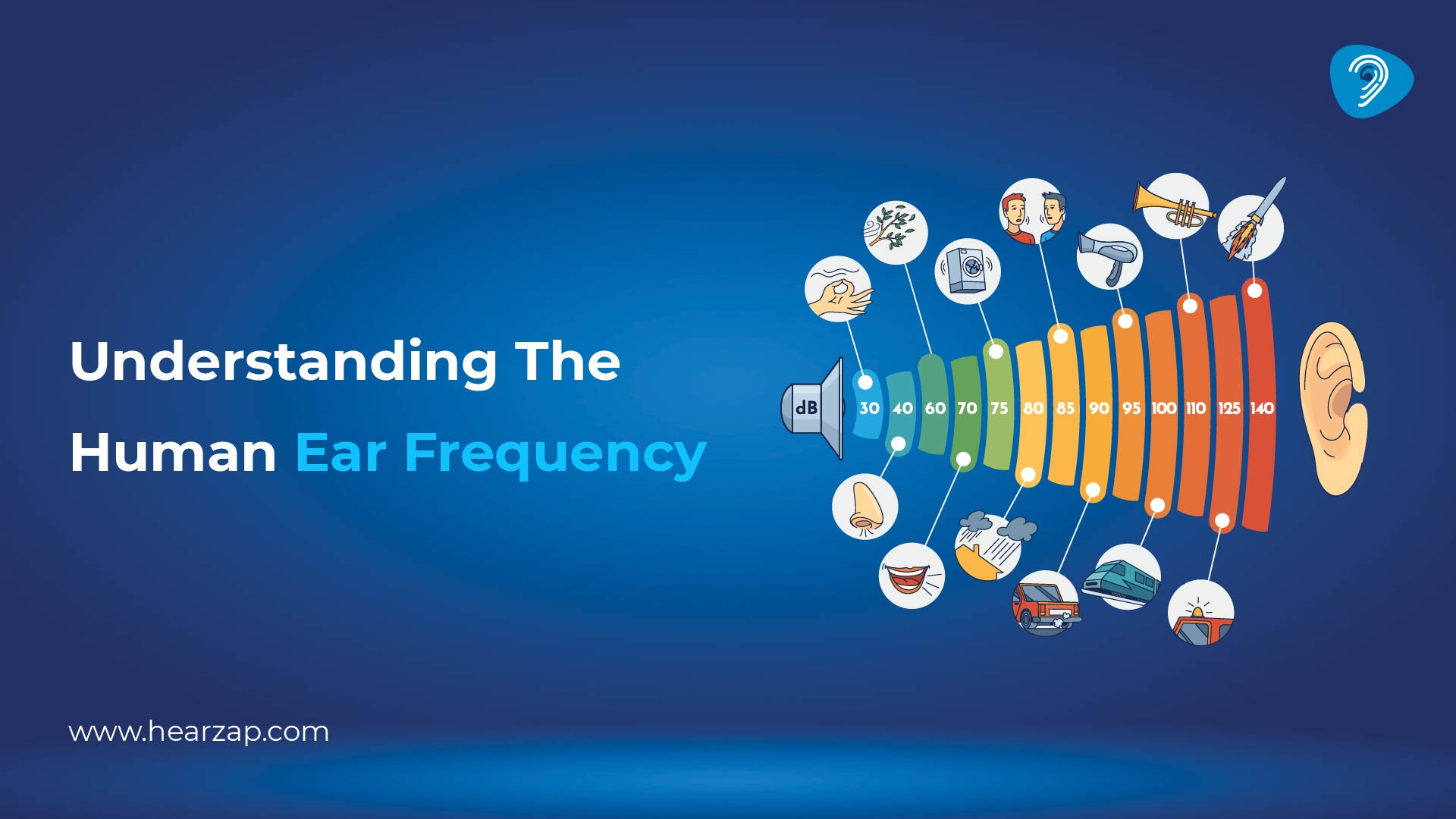
- Muffled hearing or temporary hearing loss from fluid and swelling.
- Headache, a sense of fullness, or trouble wearing glasses because the arm presses on the sore area.
Any sudden change after a week of cold-like illness, or symptoms that return soon after improving, is practical signs of mastoiditis checklist to share with an ENT.
Types of Mastoiditis
Mastoid disease does not behave the same way in everyone, so doctors group it into two broad forms.
Acute mastoiditis
Acute mastoiditis develops quickly, usually within days of a painful ear infection. Pus can collect in the air cells, forming small pockets that press on the thin bony walls. The ear sticks out slightly, the skin behind it looks red and puffy, and fever is common. Children may pull at the ears or wake at night because of ear pain. With timely ear treatment, improvement can be steady, and complications are less likely.
Chronic Mastoiditis
Chronic or recurrent mastoid disease builds slowly over months. Scarring, persistent fluid, or a small growth called cholesteatoma can interfere with drainage. People notice repeated discharge, blocked ears, or on-and-off discomfort rather than high fever. Hearing can fluctuate. It needs careful examination to protect the delicate structures of the middle ear and to plan targeted mastoiditis treatment when required.
How is Mastoiditis Diagnosed?
Diagnosis starts with a good story. Your doctor will ask about recent colds, ear infection episodes, antibiotics used, and any history of middle ear infections in childhood. During the exam, the specialist looks at the outer ear, the skin behind it, and the ear canal. Using an otoscope, they inspect the eardrum for redness, bulging, perforation, or discharge. They may gently puff air to see how the eardrum moves, or use tympanometry to test ear pressure changes.
When the picture is unclear, a hearing test helps document how sound travels through the middle ear. Blood tests can show signs of inflammation. If there is strong swelling or concern about deeper spread, imaging such as a CT scan maps the mastoid air cells and shows pockets that might need drainage. An MRI is sometimes used when soft tissue detail is important. These steps help the team confirm mastoiditis and choose safe next steps.
Mastoiditis Treatment Options
Decisions are individual, but most plans begin with medicines. A doctor may prescribe antibiotics that target the common bacteria behind ear infection and mastoiditis. These can be oral tablets or, when symptoms are severe, a short course given through a vein. Pain relief, rest, and fluids support recovery. If pressure in the middle ear is high, the specialist might place a tiny ventilation tube through the eardrum to drain fluid. In some cases, a small cut in the eardrum (myringotomy) allows pus to escape and pressure to settle.
When imaging shows a walled-off pocket or when symptoms do not settle, minor procedures can help. Suctioning discharge, cleaning the ear canal, or guided drainage of the mastoid air cells may be suggested. If the disease has damaged bone or does not respond to medicines, surgery called mastoidectomy removes the infected air cells and creates better ventilation. All of these are forms of mastoiditis treatment that aim to clear the infection and protect hearing.
Alongside procedures, ongoing ear treatment focuses on the cause - clearing nasal allergies, improving Eustachian tube function, or addressing a cholesteatoma if present. Follow-up visits check that swelling has settled and that the eardrum moves freely again.
Complications of Mastoiditis
Many people recover well when care is prompt. If infection lingers, however, nearby structures can be irritated. Potential problems include:
- A local abscess behind the ear that needs drainage.
- Persistent hearing loss from fluid, scarring, or damage to middle-ear structures.
- Spread of infection to nearby tissues, which can cause unwell feelings, headache, or neck stiffness.
- Dizziness or balance trouble occurs if the inner ear is affected.
- On rare occasions, inflammation can reach the lining around the brain. Strong warning signs include high fever, severe headache, and confusion. Urgent care is the right step if these appear.
This section is not meant to alarm; it simply explains why new swelling after an ear infection or ongoing discharge deserves a timely review.
Mastoiditis Prevention
Prevention revolves around everyday habits and early action. Practical ideas include:
- Treat colds and nasal allergies so the Eustachian tube functions well and the middle ear ventilates properly.
- Seek help for middle ear infections that do not settle in a couple of days, especially when there is fever or significant ear pain.
- Keep smoke away from children’s environments to support ear health.
- Stay up to date with recommended vaccines, which reduce some respiratory infections.
- Avoid inserting objects or harsh cotton swabs into the ear canal.
- Attend follow-up appointments after any ear procedure to confirm healing.
- Ask your clinician about mastoiditis prevention if you or your child has frequent infections; simple steps such as nasal rinses or allergy plans can reduce flare-ups.
Conclusion
The mastoid bone sits quietly behind the ear, but it shares plumbing with the middle ear. When infection reaches those air cells, mastoiditis can develop. Learning the early signs of mastoiditis, acting on persistent ear pain, and following through with personalised mastoiditis treatment helps people return to everyday routines. If you have recently recovered from ear infection and notice swelling, fever, or discharge, a prompt check by an ENT and a straightforward hearing test are sensible next steps.
FAQs
What is the cause of mastoiditis?
It usually follows an infection in the middle ear. Germs move from the space behind the eardrum into the mastoid air cells, where inflammation and pus can build. Blocked Eustachian tubes, repeated infections in childhood, and delayed care for ear discharge increase risk.
What is the best treatment for mastoiditis?
Plans vary. Doctors often start with targeted antibiotics and pain relief. If pressure is high or discharge persists, procedures such as eardrum drainage or ventilation tubes can help. Surgery is reserved for pockets that do not clear or disease that keeps returning.
Can mastoiditis lead to complications?
Problems are less common with timely care, but they can include persistent reduced hearing, abscess behind the ear, dizziness, or spread to nearby tissues. Severe headache, high fever, or confusion are urgent warning signs.
When should I see a doctor for mastoiditis?
Seek a review if there is a new earache, swelling or redness behind the ear, fever, discharge after a recent infection, or symptoms that return after seeming to improve. Children who wake at night because of ear discomfort also benefit from assessment.
How is mastoiditis diagnosed?
Doctors listen to the history and examine the ear and eardrum. They may test ear pressure and movement, arrange a hearing assessment, order blood work, and use imaging such as a CT scan when needed. These steps together confirm the diagnosis and guide care.
Contact us
We are here for all your hearing needs, from hearing tests to hearing aids. Fill out the form below, and we will give you a call soon.
Please enter a valid mobile number with 10 digits.
Recent Blogs
By None | Jan. 20, 2026
By None | Jan. 12, 2026
By None | Jan. 6, 2026
By None | Jan. 5, 2026
By None | Jan. 2, 2026